Fortuna's Russell Gorden is no stranger to hospitals or specialists. Since being diagnosed three years ago with cancer of the eye, Gorden has undergone 22 surgeries -- the first of which removed his eye, ostensibly to solve the problem -- and seen at least that many specialists.
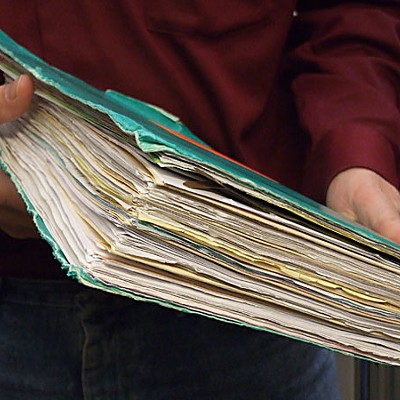
"When all of this started, there was a lot of talk about electronic medical records, but to me, it's relatively new and you still have to have a paper trail," Gorden said. He was taking a break from the cabinetry work for his wife's new martial arts studio above Body Works.
"The medical facilities, even the large ones I've been to, don't have the ability to pull everything onto their systems," he said. "I take some records with me all the time."
"He's been doing it for years, crisscrossing the country for care, with about 50 MRIs and 70 CT scans," said Dr. Mark Phelps. Phelps is Gorden's primary care doctor in Garberville; Dr. Takami Sato is his main specialist in Philadelphia.
"His files are about a foot thick," Phelps said. "All the scans, all the medications he's had -- he's been on some odd combinations of stuff, some of which is counterintuitive. Talk about someone for whom electronic medical records would be a blessing -- it changes all of that."
It would change things for Phelps, too. Now, he collects and files all of Gorden's data, some of which Phelps may not be aware exists. He weeds through, takes apart and copies key parts of "cumbersome" paper charts to barrage a new specialist with the supporting data needed for referral. All the time, Phelps worries he missed something in the file that could make the difference.
"It's uncompensated work that's very people-heavy," Phelps said. "Clicking is so much easier."
It's the quietest revolution you've never heard of, but the move to electronic medical records -- a federally mandated adjustment in the nation's health care system -- is well underway in Humboldt County. From Eureka Internal Medicine to St. Joseph Hospital, from United Indian Health Services to the Open Door Community Health Centers, from Garberville to Blue Lake, Humboldt County is emerging as a national leader in the use of information technology to revolutionize care in rural settings.
With an EMR, pertinent tests are a few mouse clicks away; so are historical comparisons of something like cholesterol numbers. Medication lists come with safety protocols. If a provider orders an uncommon dosage or prescribes something that is contraindicated because of allergy or adverse combinations, then a warning screen follows.
The hope is to reduce costs, limit medical errors, and improve quality by making paper charts passé and individual electronic medical records as secure and interoperable as financial records in the banking system. Health information technology also enables patients to manage their own care in ways not possible with paper systems.
It's already changed the way Gorden receives care.
In a two-month period in the fall, he made seven trips to the radiation oncology unit at St. Joseph Hospital. He thought it "hilarious" to watch doctors and nurses walk around with their arms at 90-degree angles and one of their hands straight in the air.
"In the crook of their arms is a laptop with the screen at eye level," he recalled. "They walk around like it's another appendage."
"It's like I'm two different people -- the image on the computer and me in the office. They're spending time with both. You may only get half the time with them looking at you, but you used to have to deal with them reading something while you talked to them."
In 2004, former President George Bush issued executive Order 13335, setting 2014 as the deadline for all Americans to have a personal electronic health record. By 2007, 43 percent of Americans knew of the ongoing effort to create a nationwide health information network, but 63 percent had never heard of electronic health records, which are the precursor to creating that system.
Physicians are split over the ease of clicking through a system some say is made more for auditors, billers and schedulers than physicians, many of whom grew up in a world where typing was someone else's job. There are fears the cost and transition will drive clinicians out of practice in an area where the average age of a primary care doc is 54.
"Computers inevitably crash, finding data can be problematic, and we're still driven to distraction by those pesky reminders," wrote Dr. Steven Kamelgarn in a December 2009 opinion piece for the Humboldt-Del Norte County Medical Society Bulletin. "EMR is a technology whose time hasn't come."
Phelps is one of many physicians who see the computer as a distraction; something that interferes with his focus on the patient and adds time at the end of a day to type notes that used to be sent out. He doesn't use an EMR during appointments -- he doesn't even use e-mail -- but doesn't see the point of arguing against a technology second-year med students such as his daughter see as a given with so many potential benefits.
What's clear is that soon there will be no paper records at all.
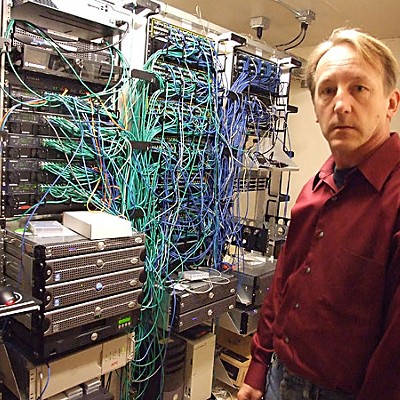
For the past two years, Eureka Internal Medicine has been scanning every paper in every patient file to complete the historical records for its new EMR. The firm has already started shredding the paper files. Records are backed up on off-site servers. Nothing is written down in a paper chart anymore.
"I don't want to go back to paper, but I'd never want to join up with a firm that's in transition," said Dr. Bruce Kessler, a 62-year-old primary care provider at the office. "It's painful."
Margot Julian doesn't want to go back to paper either. She copes with diabetes and other health challenges as a patient at Eureka Internal Medicine. "My glucose meter can plug into the computer and produce wonderful graphs that show all sorts of things," she said. "It can show information by meals -- trends at breakfast compared to trends at dinner."
A retired nurse, nursing home administrator and computer retailer, Julian likes how Eureka Internal mounts computers in a way that allows clinicians to see the patient while typing or clicking. "My husband goes to the VA and they have them mounted in cabinets and the doctor types with his back to the patient," she said. She thinks computer positioning, provider typing, security and interoperability will improve.
"There's no question: With legibility and the ability to transmit, the EMR trumps paper records in every way," she said. "But I worry about compatibility and whether it will be like the beta videotapes, where someone wins out."
Moving records to the network not only increases communication between patient and physician, but between the physician and all the other components of the health care system. St. Joseph Hospital has an established electronic interface with Eureka Internal Medicine; when Kessler arrived to work one morning in December, he booted up his in-box to see physician notes and tests for one of his patients who made an unexpected visit to the cardiologist the night before.
Dr. Jennifer Betts is the medical director of United Indian Health Services. Computers weren't part of medical school when she graduated in 1997. Now, she can't imagine good health care without them.
"It's changed our process and the way we operate," she said. "It will be transforming."
UIHS serves 7,600 Native Americans at the Potawot Health Village in Arcata and branch sites in Smith River, Trinidad, Weitchpec, Klamath and Fortuna. Now in their fourth year of use with the NextGen software system, Betts and electronic health records manager John Wiesendanger are only beginning to grasp the possibilities for a Native American population that in 2008 had its deceased average 61.8 years of age -- a decade less than the county average.
"We can start focusing on preventive care; on keeping all of our patients on the radar rather than dealing only with those who come in the office when something's wrong," Betts said. "I will never go back to paper."
"They are doing incredible things," Community Health Alliance executive director Laura McEwen said. Among them: assessments of population diseases and trends that can be customized by physician, locale or age, and individual reminders for dozens of preventive care behaviors. In the works: a health portfolio review with an action plan and advisor.
"Studying data is so powerful," Wiesendanger said. As an example, he pointed to asthma in children and adults, which "jumped out head and shoulders above everything else" after UIHS studied its health issues. In response, a primary care physician in Del Norte County is tasked to asthma care. That work will inform the reminders and protocols to be built into the system, which can then spit out which providers are doing or prescribing what.
"It's not about good doctors and bad doctors; it's about the systems in which they work," said Martin Love, chief executive officer of the Humboldt Del Norte Independent Practice Association. "We won't get much better care until the systems get better."
Locally, UIHS and the IPA are the system's leaders.
"It's monumental," said Jerome Simone, the UIHS executive director. "And I don't want to think about what it costs or I'll have a heart attack."
Thanks to the American Reinvestment and Recovery Act of 2009, Simone may now have a chance to recoup some of that investment. The Obama Administration set aside $19 billion in incentives to office-based physicians who put certified electronic health records to "meaningful use." At the beginning of next year, providers could receive up to $44,000 in Medicare funding ($48,400 for those practicing in rural or underserved areas) or $64,000 in Medi-Cal funding. Medical practices that have not made the switch by 2015 will be penalized with up to 3 percent decreases in reimbursement. There are additional incentives for hospitals, and the promise of more to come in the years ahead.
So far, the government's definition of "meaningful use" includes using EMR software at the point of care, prescribing medications electronically, implementing a system that assures interoperability or data sharing of health records and using a system capable of clinical reporting.
The local community has electronic prescribing covered. Now the focus is to help small practices convert, use electronic referrals to order tests and x-rays and confirm appointments are made and kept, said Ann Lindsay, Humboldt County Public Health Officer. She is the past president of the California Public Health Officers Association, an Arcata primary care physician and a member of the state health information technical advisory committee that is exploring "meaningful use."
"We're taking baby steps," Lindsay said. "It takes a long time to transition to an EMR, and it isn't in itself a timesaver. But if we can hook into an exchange of information that is secure and appropriate, it can help patient care. What we have to figure out is: What is going to make it easier for whatever stage people are at?"
Lindsay is a member, and Kessler the president, of the Independent Practice Association, which services 200 providers of managed care across two counties. IPA CEO Love estimated 38 percent of those providers have adopted electronic medical records compared to roughly 20 percent nationwide -- and the latter includes urban centers.
With the IPA and Humboldt County's biggest players -- Eureka Internal Medicine, Eureka Family Practice, Open Door, United Indian Health and the Veterans Administration Clinic -- leading the way, roughly 50 percent of Humboldt County residents now have an electronic medical record managed and stored by their providers. Love said another three to four practices are looking at EMR products, and 10 to 15 are interested in IPA helping them with the transition.
"We're way ahead of the rest of the country," Love said. "My phone rings constantly."
In 2003, the IPA cut its teeth on a diabetes registry, which helps area clinicians track preventive needs and treatments for those patients. That registry led to exchanges of information, performance data, and treatments that laid the groundwork for what Love calls a "sea change" in the last 12-18 months.
"There's recognition that physicians and practices were very isolated," he said. "They don't know what everyone else is doing. So we've had meetings and brought in speakers and colleagues to give them examples of what systems can do."
The IPA must be doing something right. In statewide pay-for-performance measures released early fall, it was in the top 20 percent for overall performance in measures related to clinical quality, patient experience, information-technology-enabled systems and coordinated diabetes care.
With the exception of two or three others, big name command-and-control systems filled the top quintile, making the loosely aggregated IPA crew a curiosity. While the focus often seems to be the big systems and urban centers, Love said most health care in the U.S. is provided by practices with four or fewer providers.
"Whatever health care is going to be at some time in the future, people can't ignore the fact that the majority of the country looks more like us than the others on that list," he said.
Harry Jasper is lean, young and dressed with the professional style that is the exception rather than the rule in Humboldt County. It is Dec. 2 and his presentation on personal health records is an agenda item at the monthly meeting of Southern Humboldt Working Together.
Fifteen people -- all but two with coats and six with mufflers wrapped around their necks -- gather around a horseshoe table in an unheated room of the Sanderson Building across the street from Garberville's spanking new city center plaza. Curtains hang unevenly -- none are fully attached to their rods. The light fixtures are in similar condition.
"Are we the healthiest community possible?" asks Jasper, the administrator for the Southern Humboldt Community Healthcare District. "Do we have health care or sick care?"
Jasper believes personal health records will be the catalyst to transform the system as debit cards transformed banking, e-mail altered communication, and digital cameras revolutionized photography. In December, he submitted a $75,000 grant request to fund an effort to introduce personal health records to southern Humboldt.
The difference between an "electronic medical record" and a "personal heath record" is the ownership: "It's a total shift in paradigm about who is the keeper of the medical record," Jasper said. "The patient owns it, then allows authorized, secure systems to access their secure portal of information."
Jasper and the Southern Humboldt Community Health District are looking to adopt a plan offered by a health care provider in Washington. Not everyone is so enthusiastic, though.
"I've been a skeptic since it began," Love said of the PHR movement, which took off in Bellingham, Wash. "If people won't take care of themselves, they won't take care of their record. In most configurations, they rely on an awful lot of fancy programming or manual data entry that are expensive or don't exist."
At the moment, consumers view health information technology as helpful, but not as a source of fundamental change in health care, stated the authors of a July 2009 report prepared for the federal Agency for Healthcare Research and Study. "They tend to view health IT as being solely the domain of providers," the report stated.
That's a mistake, Jasper said. Providers have a need to make notes and keep records about a patient, but patients need to manage health issues and plan ahead for emergencies by taking control of their health and records.
"When they rolled out a PHR in Washington, patients were asked to grant prior authorization to the emergency medical services system," Jasper said. "A 911 call comes in and the paramedics can access that PHR before they get to the house."
Paramedics and the hospital ER know about allergies and medications, and would also know about advance directives, even if the patient is unconscious. That saves time and lives, Jasper said.
"The patient may or may not grant access," Jasper said of the choice to pre-authorize. "Right now, there isn't any access at all so any step in the right direction is progress."
St. Joseph Hospital is already making use of personal health records for its Care Transitions program. Created in spring 2007, senior level nursing students from Humboldt State University provide individual coaching about disease management to people moving from the hospital to home. It's based on the MyVIA program, which was developed for a farm worker population that shifts providers with the crop season.
The Care Transitions PHR is a Web-based portal that is primarily focused on medication reconciliation. A medication adjustment made at the primary care provider's office is updated on the PHR. The patient can then allow that adjustment to spread throughout his network of providers. "If the person ends up in an ER, he can let people log on to see the update," Starr said.
Care Transitions Program Coordinator Sharon Hunter said since the introduction in July, 13 people had opted for the computerized PHR -- a small number, considering the program manages 80 to 120 people on a continuous basis. "Anecdotally, the people who are 70 and older are saying no; the people 60 and younger are saying yes," she said. "Those who say no say they aren't interested, don't have a computer, or don't know how to use a computer."
Jack Norton, human resources manager at the Blue Lake Casino and Hotel, sees the potential for PHRs to decrease health insurance costs and improve wellness. "We think every dollar in preventive health will pay us back four to 10 times the savings in health care costs," he said. "We're willing to be on the cutting edge."
At a November health fair, the Blue Lake Rancheria's Eric Ramos and Arla Ramsey rolled out Share Your Health, a private business venture spearheaded by Jasper. Participants get a health assessment, blood pressure monitor, a scale and three fitness books -- all paid for by the company. They then share their numbers online -- anonymous posting is an option -- to create a public support group.
Norton plans to offer a monthly newsletter to share stories. Those who report their numbers are eligible for a $50 monthly raffle prize. Posting begins in January.
"I don't know if it's proven to work. I don't know which PHR is best," Norton said. "But I know chronic conditions make up about 80 percent of the costs of health care and that behavioral health is at least 40 percent of the problem."
"So far everyone really likes the idea because it keeps health in sight and in mind and everyone can see progress," Norton said.
"It was more than I expected at the Health Fair," employee Janet Brooks said. "A lot of us came just for the flu shot."
She looks forward to participating -- anonymously.
"I'm not that brave," she said.
Norton said he would like to do more. He sees Share Your Health as a customized add-on product to a PHR not yet available. "I called Microsoft Health Vault and they told us to call back when we had 5,000 people or teamed with enough employers to get that many," Norton said. "There's no free lunch. Someone has to pay for it. Down the road they may give you ads or charge a fee to maintain it."
Norton said the casino is willing to pay, just as Jasper is willing to take the lead.
"Someone has to plow the field," Jasper said.







Comments (3)
Showing 1-3 of 3