When I began my brief career as a drug and alcohol counselor (2010-2012), I had learned to define sobriety along some pretty stark lines: Either you were abstinent from all psychoactive substances or you weren't. Sober people don't take medicine that doesn't have their name on the label. Sober people don't occasionally take psilocybin mushroom to fast-track their spiritual growth. And sober people don't smoke weed, even though it's "just a plant," it's medicine and is rarely habit-forming. (Actually, it's more habit-forming than most people think, but we'll get to that later.)
These tenets were rooted in common sense and the hard-won experience of recovering addicts. As anyone who has struggled with addiction or loved an addict knows, defining what constitutes a relapse and then sticking to that definition can be very important, and blurring the lines by experimenting with any mind-altering substance or even behavior (such as sex or gambling) can lead to a full relapse with one's drug of choice. Sublime summed this up more succinctly in their 1996 song "What I Got": "I don't get angry when my mom smokes pot/Hits the bottle and goes back to the rock."
But what I found when I actually began working with addicts and alcoholics is that success in recovery often relied on letting my clients define the terms of that success. And I was lucky enough to work for a program that didn't demand our clients practice complete abstinence outside of attending our classes and therapy groups. I still recommended complete abstinence, 12-step groups and ongoing therapy, but I also learned that if clients started going to the gym instead of going to the bar, or if someone switched from methamphetamine to marijuana, and their lives improved, and they called it a win, I could call it a win, too. This philosophy, loosely defined as harm reduction, is beginning to gain more ground in addiction treatment. But most programs still use complete abstinence as the yardstick by which success is measured. (For the record, if you're an addict or alcoholic, I still recommend all of the same things I suggested when working in treatment.)
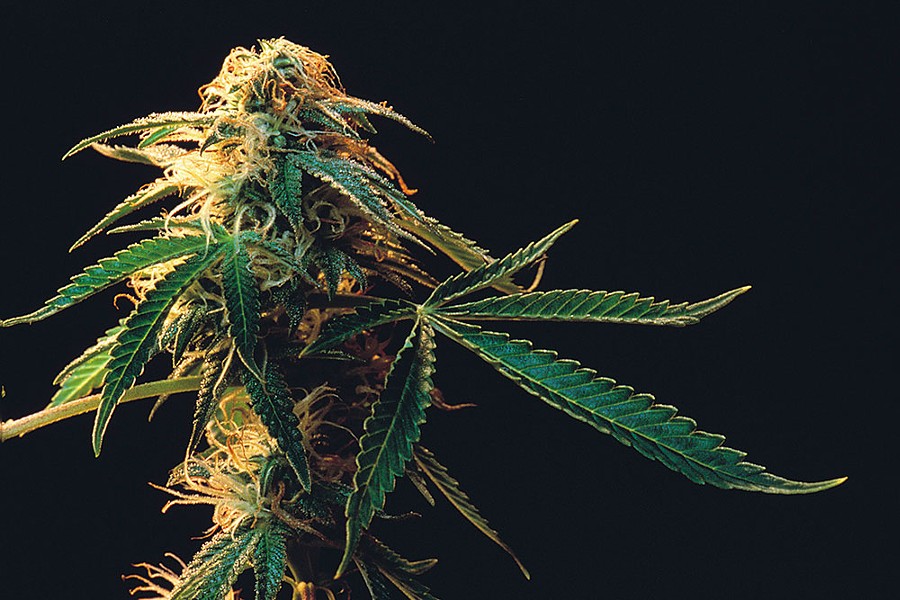
Which brings us to weed. It's a sticky topic in the recovery community, especially here in Humboldt County. The industry and recovery are often difficult to reconcile. On more than one occasion I had to ask clients to leave groups when they arrived smelling of their work, because I was worried it would trigger other group members. I know people who have maintained a successful recovery for decades despite growing pot and others who habitually relapse because they're lured back to old friends and old habits during the trim season. Recently, Rolling Stone ran an article about medical marijuana and its lack of acceptance in the recovery community. Although federal regulations have prevented extensive study and approval by the Federal Food and Drug Administration, cannabinols have been shown to help with a wide spectrum of physical and emotional problems, and their medical benefits can often be separated out from their recreational highs.
I have a couple of theories as to why there is reluctance to embrace medical marijuana in the recovery community, some of which is based on my own former ignorance. First, I think that many of us were introduced to the idea of "medical marijuana" as a backdoor way for people to smoke the stuff recreationally, before the current sophistication of strictly medicinal CBD. In line with the afore-mentioned warning about how "sober people don't take medicine that doesn't have their name on the label," recovering addicts might righteously feel dubious about using anything that requires going down to their local dispensary.
Cannabis was once a common ingredient in patent medicines, but for most of modern memory it has been a prohibited, stigmatized stoney gateway drug. I would still be reluctant to recommend its use to anyone who is in recovery. But I have also seen many people relapse and die after taking drugs that do have their names on the label, particularly opiates. Medical cannabis is now being prescribed to address chronic pain and other issues traditionally treated with highly addictive narcotics. So, should medical cannabis be formally reclassified by recovery professionals? Can it be totally separated from its relapse-triggering stoney properties? And is cannabis really addictive? Is it a gateway drug? In short order, my answers: Probably, probably not, yes and yes, but not in the way you think. Buckle up, because next week we're talking about neurochemistry.

Comments (3)
Showing 1-3 of 3